2022 was the bad year that wasn’t—at least for a mysterious paralyzing condition in children.
In the decade before, hundreds of young, healthy kids in the US abruptly felt their limbs go weak. Debilitating paralysis set in. In recent years, around half of affected children required intensive care. About a quarter needed mechanical ventilation. A few died, and many others appear to have permanent weakness and paralysis.
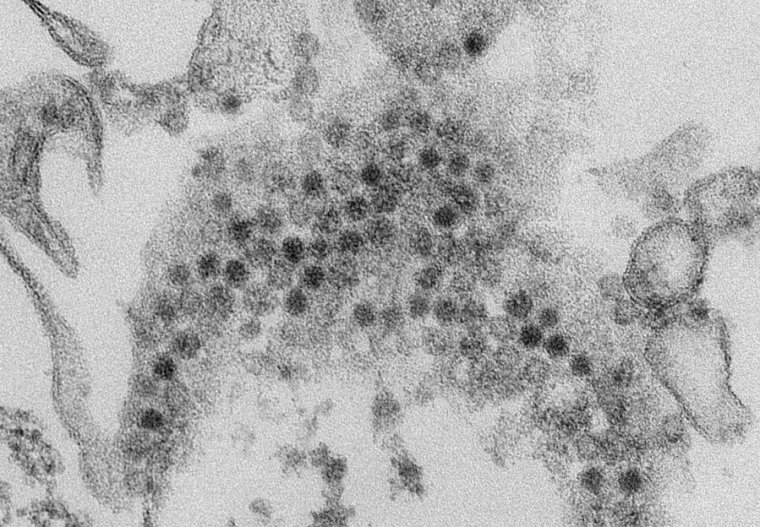
Researchers quickly linked the rare polio-esque condition to a virus known for causing respiratory infections, often mild colds: enterovirus D68, or EV-D68 for short. Identified decades ago, it’s a relative of polio, one of the over 100 non-polio enteroviruses that float around. But when EV-D68 began surging, so did the mysterious paralyzing condition, called acute flaccid myelitis, or AFM. The menacing pair seemed to come in waves every other year, likely starting with a cluster of cases in California in 2012. In 2014, there were 120 AFM cases in 34 states. In 2016, 153 cases in 39 states. In 2018, 238 cases in 42 states. By contrast, there were just a few dozen cases or so in each of the years in between, cases that were sporadic or unrelated to EV-D68.
2020 was the next year to watch, but SARS-CoV-2 came crashing in. Amid shutdowns, masks, distancing, and heightened hygiene, the pandemic obliterated normal transmission cycles of many other pathogens. EV-D68 was no exception. So researchers looked to 2022. At that point, there would be a four-year gap since the last EV-D68 surge, not the normal two-year gap. The pool of young children who had not been exposed to a recent wave of EV-D68 would be even larger than usual. They seemed like sitting ducks.
“Although the exact timing of the next enterovirus D68 outbreak is difficult to predict, large outbreaks of enterovirus D68, and therefore acute flaccid myelitis, are likely to be imminent,” US researchers warned in a commentary published in The Lancet Microbe on January 7, 2022.
In the summer, EV-D68 began rising. Its spread looked to rival what was seen in 2018, when there were 238 AFM cases. The EV-D68 strain circulating was similar to the 2018 strain, too. In early September, the Centers for Disease Control and Prevention sent a warning to clinicians through its Health Alert Network: EV-D68 is rising around the country. Be on the lookout for AFM. It’s coming.
But it never came. Though the EV-D68 wave came and went, AFM cases stayed low. Looking at the percentage of kids with a respiratory illness who were positive for EV-D68, transmission in 2022 appeared to be even higher than it was in 2018. As expected, the virus came roaring back after its pandemic break. But there were only 47 cases of AFM that year, not hundreds. It was an off-year for the condition.
So what happened? Why didn’t AFM surge along with EV-D68? In short, no one knows.
Pleasant surprise, lingering mystery
“It’s surprising, totally,” Matthew Vogt, a pediatric infectious disease expert at the University of North Carolina, Chapel Hill, told Ars. He noted that he was among the authors of the January 2022 commentary in The Lancet Microbe. “I was on record, really thought I understood what was happening, and I was wrong… I thought we were going to have a bad outbreak in 2022.”
It’s yet another riddle swirling around AFM. Why did EV-D68 start causing national surges in 2014? Why do most children with EV-D68 get a mild respiratory infection and recover, while an unlucky few develop paralysis in the days afterward? And a pressing question now: What comes next?
In May of 2022, Vogt, along with colleagues, published damning evidence that EV-D68 is behind some AFM cases. The study, appearing in the New England Journal of Medicine, found genetic material (RNA) and proteins from EV-D68 in motor neurons in the spinal cord of a 5-year-old boy who tragically died of an AFM-like illness in 2008. Until then, the virus had been hard to pin down in the central nervous system, rarely showing up in cerebrospinal fluid—which is the case for polio virus as well.
Vogt says he’s now bracing for a possible surge of AFM this year, 2024, the next surge year if the every-other-year pattern returns. Modeling suggests EV-D68 won’t surge quite as strongly as it did in 2022 but will have a wave. Vogt is cautious, though. “If I’ve taken anything away from respiratory virus circulation ever since the pandemic, it’s that if we think we can predict anything, we’re probably playing a fool’s game,” he said.
Kevin Messacar, a pediatric infectious diseases expert at Children’s Hospital Colorado and another co-author of the January 2022 commentary, agrees. “The decoupling of AFM and the potential of AFM returning with an EV-D68 spike, I don’t think anyone can predict at this point,” Messacar told Ars. Instead of trying to predict, he said, it’s better to prepare.
Last Thursday, researchers at the CDC published something akin to a post-mortem of the 2022 outbreak that wasn’t. The analysis carefully combed through the AFM surveillance data from 2018 to 2022, trying to help understand what happened in that latter year. It provides new insights into the cases and ways to sharpen responses. For instance, over half of all the AFM cases in those years first presented at emergency departments—thus, emergency department doctors are key frontline workers to target for outreach during potential AFM surges. And although there was a relatively small number of AFM cases in 2022, those cases looked more like the cases in the surge year of 2018 than the cases in 2019 through 2021.
In the 2018 and 2022 AFM cases—which both coincided with EV-D68 waves—children with AFM were more likely to have had an illness with a fever recently; have upper-limb weakness rather than lower-limb weakness; and have immune cells in their cerebrospinal fluid. Basically, AFM triggered by EV-D68 appears to have a distinct clinical profile than AFM caused by other viruses and conditions, the CDC researchers concluded.
Shifting viruses
The researchers also highlighted the two leading hypotheses of why 2022 wasn’t an AFM outbreak year. One is that something about the virus changed to make it less likely to move into the central nervous system. “[P]ossibly, EV-D68 viruses circulating in 2022 were less neurotropic or less likely to cause neurologic disease than were viruses circulating during 2014, 2016, and 2018,” wrote the CDC authors, led by epidemiologist Erin Whitehouse of the viral disease division of the CDC’s National Center for Immunization and Respiratory Diseases.
There’s some evidence that this is possible, Kenneth Tyler, chair of the neurology department at the University of Colorado School of Medicine, told Ars over email. Using EV-D68 virus isolates from 2014, studies by Tyler and colleagues found that some viruses are better at infecting the central nervous system and causing paralysis in mice than others. The critical differences, Tyler said, appear to be in a specific viral protein, called VP1, which is involved in helping the virus get into human cells.
“It is a testable idea to see whether the 2022 strains have lost or retained neurovirulence and, if lost, whether there are identifiable changes in VP1 (or other proteins) that might explain this,” he said. And, he added, there’s a reasonable evolutionary explanation for why this could happen: EV-D68 doesn’t have anything to gain from infecting the central nervous system. It’s a dead-end, and, if anything, it makes transmission more difficult for the virus, given the debilitating effects on its victim. “It is possible that the virus has evolved in a way that makes it less neurotropic while still preserving its capacity to cause respiratory disease,” Tyler said.
Variability in causing paralysis is also seen with polio viruses, Messacar pointed out. There are three strains of wild polio virus (type 1, 2, and 3), and each has its own predilection for causing paralysis. (Type 2 and 3 have been eradicated, but type 1 and vaccine-derived strains remain.) The CDC notes that paralysis occurs in about 1 out of 200 to 1 out of 2,000 cases, depending on the strain.
It’s possible that certain mutations could directly help viruses move into the central nervous system more readily, but Messacar noted that it could also be less specific than that. Some researchers suggest that EV-D68’s jump to causing AFM a decade ago may have to do with high viral loads. Researchers in Europe have suggested that some of the more recent EV-D68 strains are more likely to replicate and transmit at higher quantities. That hefty load of virus may be more likely to spill over from the respiratory tract to the central nervous system, leading to paralysis.
For now, there are no clear answers on any of this. The EV-D68 strains circulating in 2018, when there was an AFM surge, aren’t massively different from what was circulating in 2022, Vogt said. Researchers around the world have “analyzed the bejesus out of these [virus genetic] sequences.” But so far, “there is no smoking-gun” mutation that explains the abrupt emergence or puzzling absence of AFM surges, he said.
Shifting immune responses
The hypothesis Vogt favors is the second one the CDC highlighted: Instead of something in the virus changing, it was something in the kids. Specifically, an onslaught of respiratory infections in 2022 could have revved up children’s immune responses, which in turn prevented EV-D68 from progressing to neurologic disease and paralysis—aka the viral interference hypothesis.
2022 was a blockbuster year for respiratory viruses, generally. SARS-CoV-2 was still circulating widely, and influenza and RSV (respiratory syncytial (sin-SISH-uhl) virus) made roaring comebacks. The idea is that if you have a viral infection right before being infected with another virus, innate immune responses are still ramped up above baseline. Those responses could have helped keep EV-D68 in its place—the respiratory tract—and out of the central nervous system. Vogt says he has some preliminary unpublished data that supports this hypothesis. It’s preliminary data, Vogt cautioned, but it also just makes sense with what we know innate immune responses can do. “It’s not that earth-shattering.”
Viral interference is my “favorite hypothesis of the moment,” Vogt said. “I really like that idea that there were so many viruses circulating at that time that a lot of these kids probably had their defenses already up.”
“I’m not sure I buy that argument,” Messacar countered. He noted that EV-D68 seemed to start rising before RSV and influenza. But perhaps more puzzling, he wondered, if children’s immune systems were already ramped up, why was there still a spike in EV-D68 respiratory infections? If you had elevated innate immune responses, “potentially you wouldn’t see the respiratory cases, either,” he said. Messacar and his colleagues are working to separate out the immune responses that fight EV-D68 respiratory infections from those that fight EV-D68 neurologic disease.
While researchers explore the various hypotheses, they all suggest it’s most likely a combination of them that is playing a role in all the unanswered questions. The virus is constantly changing, and children’s immune responses are constantly changing. The viral landscape is constantly shifting. Some children may have silent genetic predispositions for AFM.
As research continues, we should still prepare for the next AFM surge—whenever that may be, the researchers said. It’s critical for front-line workers to identify cases promptly because many children progress to respiratory distress and should be admitted to the hospital for monitoring in case that happens. It’s also critical for collecting the right samples, such as respiratory swabs, needed to help piece together answers.
“One season where it didn’t align—that’s not enough at all for us to just lower our guard,” Vogt said. “We would be foolish, absolutely foolish, to let our guard down … I hope I’m wrong again, I really do, but I wouldn’t want to be caught unprepared.”